Recognizing the signs of postpartum depression
[ad_1]
High school sweethearts Mitchail and Brenda Encarnacion filled the early years of their marriage with excitement, before embarking on another kind of adventure. According to Mitchail, Brenda was “gung-ho” about the impending birth of their baby. “She was reading all these books. It was, like, YouTube videos. She made me a PowerPoint! It was like a full-time job for her,” he said.
In October 2020, Brenda gave birth to their daughter, Evelyn. Yet, despite all their preparation, there was one thing they didn’t see coming. “Sometimes, I’d catch her just, like, crying for no reason,” Mitchail said. “And I would always ask her, and she’d be like, ‘Yeah it’s just hormones.’ She just kept calling it ‘Mommy brain.'”
As a paramedic, Mitchail said he recognized the signs of postpartum depression, and encouraged her to see a therapist, but says things didn’t improve. “The morning before, she looked different,” he said. “I could see it in her eyes that there was something wrong.”
That day, nine months after giving birth, Brenda Encarnancion took her own life. She was 30 years old.
Family photo
According to the Journal of the American Medical Association, in the United States, one in seven women experiences postpartum depression (PPD). More new moms die from suicide or overdose than anything else.
“Their main complaint is, ‘I’m feeling overwhelmed,’ and that should really be a signal for us to dive deeper,” said Dr. Kristina Deligiannidis, director of women’s behavioral health at New York’s Zucker Hillside Hospital. She researches and treats depression in pregnant and postpartum women.
She said PPD is not the “baby blues.” “They both exist, and that’s part of the confusion,” Deligiannidis said. “The baby blues are really this normal physiological adaptation to delivering a baby. And so, our brain needs to reset, and sometimes that can affect our mood. And it never lasts more than two weeks, does not require any treatment at all.”
Postpartum or perinatal depression does not go away after two weeks – and the symptoms are often more severe than feeling a little sad. “Many women will withdraw from the things that they used to enjoy,” Deligiannidis said. “They’ll also report just feeling drained of energy.”
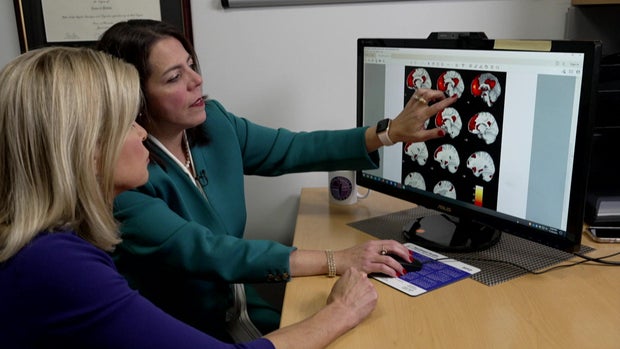
PPD is triggered by factors like genetics, stress and changing hormones. You can actually see it when looking at scans of the brain’s medial prefrontal cortex, which is important for emotion regulation and cognition. “This is the area that we’re finding really has much more activity, more fired up in postpartum depression, than in women without any symptoms at all,” Deligiannidis said – evidence that PPD is real, and which dispels the stigma that this isn’t a “true” medical illness.
CBS News
Lisette Lopez-Rose didn’t need a brain scan to tell her something was wrong. “I like to use the analogy of shells, like a crab shell,” she said. “I felt like, you know, the meat is the baby, it was picked out, and then I’m just discarded. That’s really how I felt.”
In the months after she gave birth to daughter Sybil in November 2020, Lisette began to have suicidal thoughts. But her doctors never knew. “Everything’s about the baby, and it’s never about the mom,” she said. “It’s never about, like, how am I doing? So, I never had a conversation. I think if I did, I might’ve been a little bit more truthful.”
She said she was afraid of admitting that she did not feel fine. “I’m a woman of color, I’m Latina. If I say something like ‘I want to take my life,’ or something like that, I feel like they would’ve taken my baby away. That was my mentality, and that’s why I was not honest about disclosing how those thoughts were affecting me.”
Lisette eventually found help, and now shares her journey on social media, hoping to destigmatize PPD.
But experts say only about six percent of diagnosed women receive treatment, and thousands more never come forward at all. “I think we’re likely underestimating the population that’s suffering,” said Joy Burkhard, executive director of the Policy Center for Maternal Mental Health.
The reason so many women fall through the cracks, she said, is that in the United States, women are frequently passed from one health care provider to another. “Our system doesn’t hold any one provider responsible for maternal mental health disorders,” Burkhard said. “The problem really lies in accountability. Who’s responsible for detecting and developing some treatment plans to support women?”
Traditional treatments, like antidepressants, take time, something new moms don’t really have. But starting this week moms may have another option: a new FDA approved drug, Zurzuvae, the first-ever pill specifically for postpartum depression.
Dr. Deligiannidis ran one of the trials, and says the pill, taken for 14 days, provides almost immediate relief. That quick reaction, she said, gave her goosebumps: “It was a little unreal. We just aren’t trained in this way, to think our therapies can work this quickly.”
The overall price tag on the treatment is around $16,000, and it’s unclear at this time if or how much insurance will cover. There are other unknowns as well; Deligiannidis said it should not be taken while breastfeeding: “We just don’t have data, because it’s not even out yet. We don’t know if there are effects on the baby. In time, we’ll have, you know, information to help patients who are lactating make those decisions.”
But experts like Joy Burkhard say it’s a reason for hope: “It’s a game-changer. But what we don’t want to overlook is the fact that women still need support. We need the pill, but we need much more.”
Mitchail Encarnacion likes to share happy memories with his daughter, Evie. But he’s willing to talk about the painful ones, too, with the hope that, by looking back, he can encourage more women with PPD to come forward.
“I didn’t think it would happen to me,” he said. “I didn’t think it would happen to somebody that happy. If these people knew, they’d still have their mom. ‘Cause now all Evie has is pictures of her.”
CBS News
For more info:
Story produced by Sara Kugel. Editor: Carol Ross.
See also:
If you or someone you know is in emotional distress or a suicidal crisis, you can reach the 988 Suicide & Crisis Lifeline by calling or texting 988. You can also chat with the 988 Suicide & Crisis Lifeline here.
For more information about mental health care resources and support, The National Alliance on Mental Illness (NAMI) HelpLine can be reached Monday through Friday, 10 a.m.–10 p.m. ET, at 1-800-950-NAMI (6264) or email info@nami.org.
[ad_2]
Source link